PBMs are under more pressure than ever before to demonstrate the value they bring to payers, providers, and patients even while staying on top of ever-changing regulations. DrFirst’s unique expertise enables PBMs to focus on innovation while we focus on compliance, transparency, and supporting providers at the point of care.
What’s Your Biggest Challenge?
New regulatory requirements come up frequently. We have to dedicate resources to stay on top of these instead of focusing on innovations.
We’re under a lot of pressure to be more transparent, not only in pricing but also in demonstrating how we help control healthcare costs and improve patient health.
We need to tap into technology that helps us improve member experience, lessen administrative components, and put patients first.
Don’t see your challenge? Contact us.
Answer the Call
for Transparency
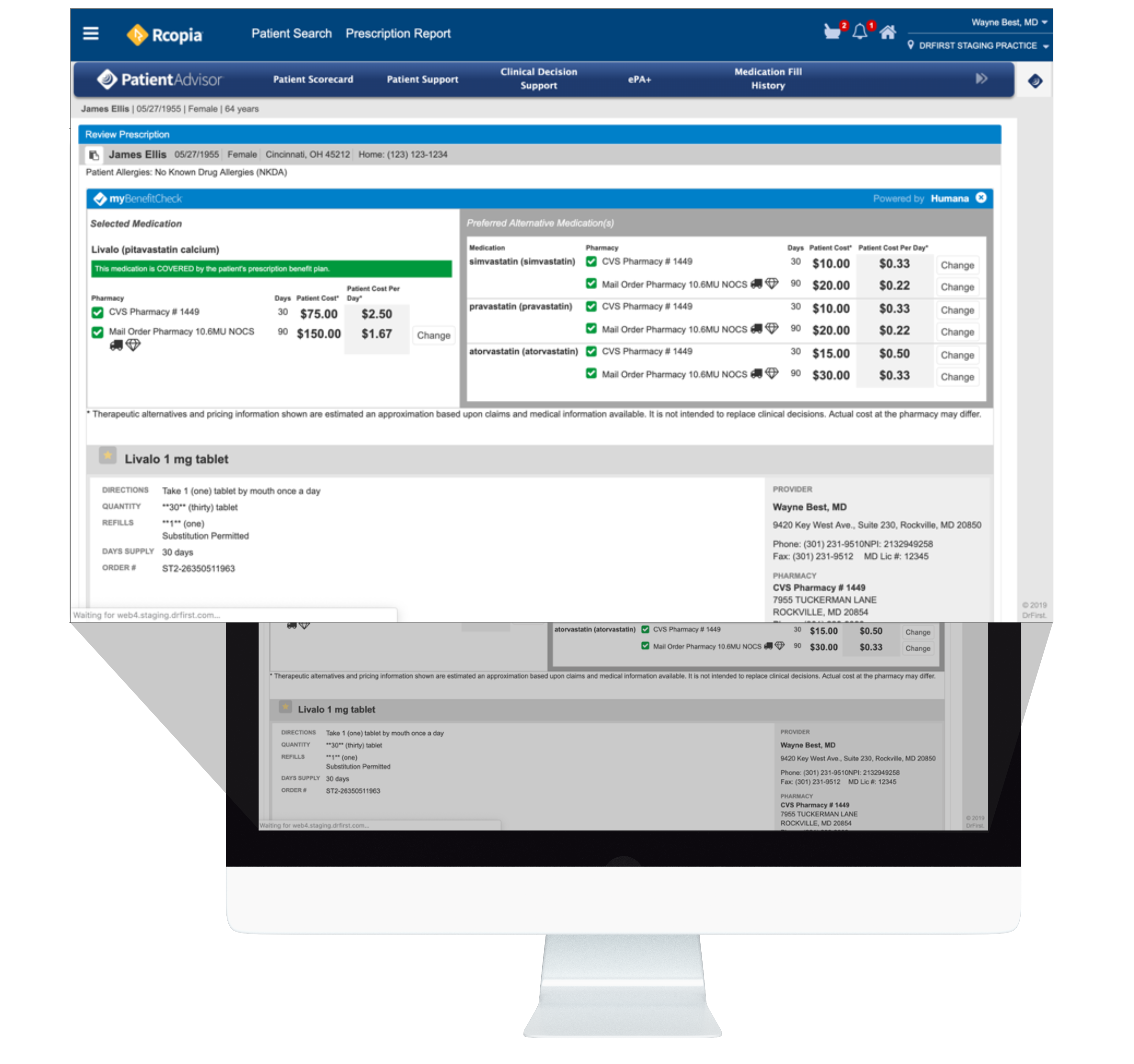
PBMs play a pivotal role in healthcare, touching nearly every prescription written through claims adjudication, prior authorization, appeals and grievances, and more. This central role has also brought intense scrutiny to PBM practices and policies, with growing requests for transparency and accountability.
We have the tools to help PBMs demonstrate the value they bring to healthcare in terms of cost-effective therapeutic options, administrative support, clinical outcomes, and digital health solutions.